Treatment of Arteriovenous Malformation (AVM)
- Surgery (Microsurgical Resection)
- Radiosurgery (stereotactic radiotherapy)
- Embolization (endovascular surgery)
- Conservative Medical Management
- Special Considerations for Treatment of Hemorrhaged AVM
- Treatment Options in Children
- Pregnancy and Treatment
Treatment is primarily aimed at prevention of new or future hemorrhage. A hemorrhage in the brain is a type of stroke in which a blood vessel ruptures and bleeds into the surrounding brain. For more information on strokes, please visit the American Stroke Association at www.strokeassociation.org .
We also encourage you to visit our support resources section for additional information and tools to help patients, and caregivers living with AVM.
Determining the best course of treatment is dependent on several factors including:
- Whether the AVM has bled before. The occurrence of a first hemorrhage is associated with an increased risk of subsequent hemorrhage. This often prompts a more aggressive approach to treatment with patients who have already had an episode of bleeding.
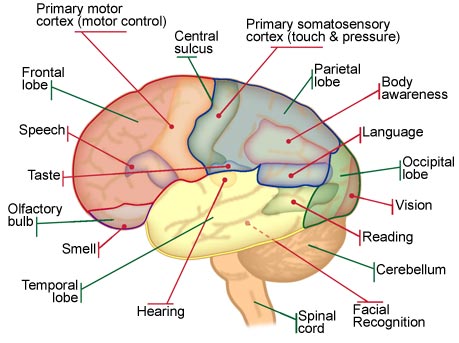
- Location. The accessibility of the AVM to surgical intervention, and specifically if the AVM is located in an area of “eloquent” brain. Eloquent brain includes areas of the brain that control speech, motor functions, or sense.
- Size. Smaller AVMs present with hemorrhage more often than large ones. In addition, smaller AVMs produce larger hematomas when compared to medium or large AVMs. A hematoma is a mass of usually clotted blood that forms as the result of a broken blood vessel. Because the brain is in an enclosed space, a larger hematoma can increase the pressure on the brain tissue, blood vessels, and spinal fluid contained within the brain. However, small AVMs are less likely to press on adjacent brain, which can cause symptoms such as headaches or seizures.
- Symptoms that it is causing. In some cases the symptoms triggered by the AVM are severe and debilitating, significantly affecting the quality of life of the patient. In other cases, the AVM is found by accident and there are no symptoms.
The risks of interventional management (microsurgical resection, radiosurgery, or embolization) vs. conservative medical management need to be weighed carefully against the expected natural course of the disease on a case-by-case basis. It is important that anyone facing the prospect of treatment make an informed choice.
The primary treatment options for an AVM include:
- Surgery (microsurgical resection) – surgery to remove the AVM from the brain.
- Radiosurgery (stereotactic radiotherapy) – multiple focused beams of radiation directed at the abnormal vessels of the AVM causes the vessels to thicken ultimately “choking off” the AVM.
- Embolization (endovascular surgery) – using the same procedure as a diagnostic angiogram (link to angiogram page), one or more blood vessels feeding the AVM are closed. This treatment is generally used in conjunction with microsurgical resection or radiosurgery.
- Conservative medical management – monitoring of the AVM with a primary focus on symptom management.
Your treatment plan may include a combination of these options. Treatment options should be carefully discussed with your doctor. The specifics of your case (such as the factors discussed above) will determine the best course of treatment that minimizes risks, and maximizes the quality of life for the individual.
Microsurgical resection is the most aggressive form of treatment, as well as the most certain treatment to completely remove the AVM. With that said, microsurgical resection is also a highly invasive procedure, and in certain cases other treatment options, or combination of treatment options, may be more effective, while minimizing risks and maximizing quality of life for the individual.
To aid doctors in making a recommendation for treatment, the Spetzler-Martin (S-M) Grading System is used to assess if the AVM is an appropriate candidate for microsurgical resection. While the primary purpose is to estimate risks to a positive outcome of microsurgical resection, the S-M Grading System is also considered a universal tool for grading AVMs.
In the S-M Grading System, the AVM is graded on the basis of:
- Size – The size of the AVM relates to the number of feeding arteries, degree of blood flow, and extent of cerebral steal.
- Pattern of venous drainage – The pattern of venous drainage relates to depth of the AVM and surgical accessibility.
- Location – How close the AVM is to eloquent brain. Eloquent brain has easily identifiable neurological function and, when injured, produces disabling neurological deficits. Eloquent brain includes areas of the brain that control speech, motor functions, or sense. Other areas of the brain involved with more subtle functions are considered non-eloquent.
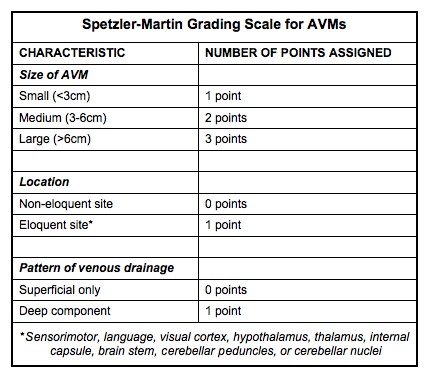
- Grade I - II malformations are generally considered operable. They are small, superficial, and located in non-eloquent cortex.
- Grade III - IV malformations require discussion on a case-by-case basis for best course of treatment. They are large, deep, and situated in neurologically critical areas.
- Grade V malformations are essentially inoperable AVMs.
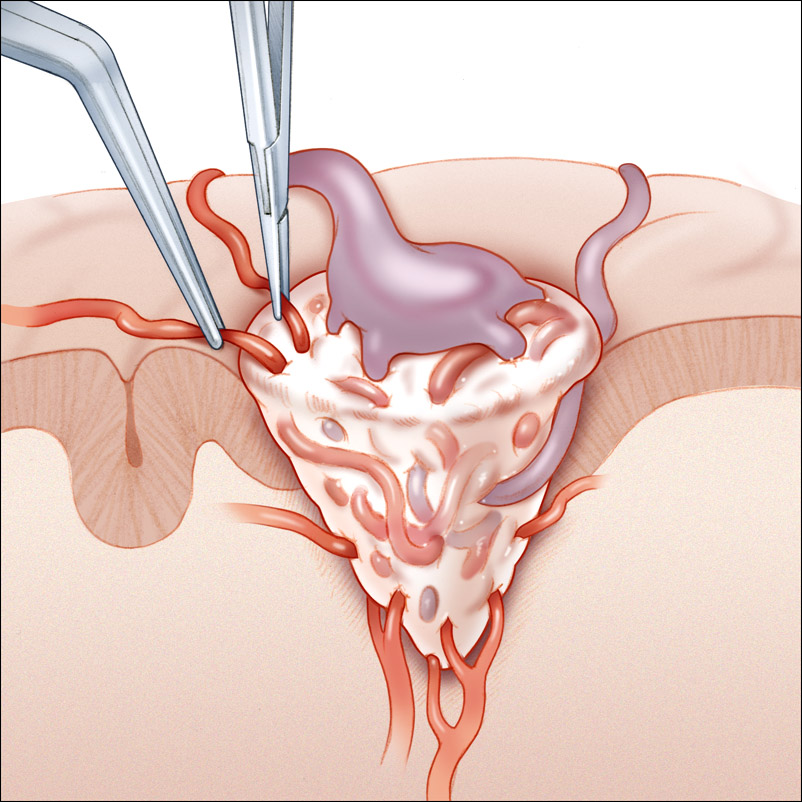
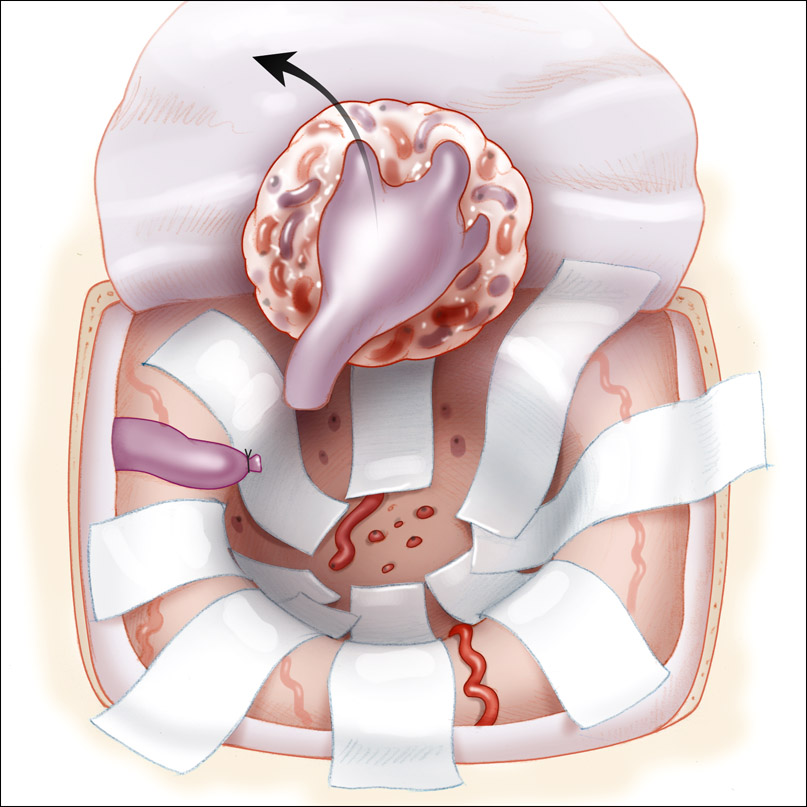
At this stage a complete state of hemostasis (stoppage of blood flow through the AVM) is critical. Bleeding arteries will obscure the surgery and/or bleed into brain tissue.
Finally the draining vein or veins are closed and separated from the AVM. The AVM is then resected (taken out of the brain). The resection bed is carefully inspected for bleeding before the surgery is finished. The bone is reattached with small metal bars and screws that are MRI compatible (titanium). The muscle is stitched. And the skin is generally either stitched or stapled.
Prior to your surgery, usually the day before, you will attend a pre-operative appointment. In the pre-operative appointment you will undergo a series of tests (blood tests, EKG, chest X-Ray, etc.) This testing is to help assess your general medical condition and that it is safe for you to undergo anesthesia and surgery.
Your neurologist will explain the microsurgical resection procedure and risks. You will be asked to sign release forms indicating that you understand the procedure and risks.
An anesthesiologist will discuss the use of anesthesia during your procedure. Anesthesiologists are doctors who are responsible for managing your medical status prior to, during, and after your surgery. It is very important for you to carefully go over any other medical conditions that you have, and to come prepared with an accurate list of any medications that you take.
Your anesthesiologist will also provide you with guidelines, such as not eating prior to your surgery.
General anesthesia (where the patient is totally unconscious) is typically used for this type of surgery. Let your doctors know ahead of time if you have a problem with recovering from anesthesia. There are medications that can assist in your recovery from the anesthesia.
After you are sedated and asleep, a breathing tube will be inserted. A catheter will be inserted in your bladder to monitor urine production.
After surgery you will be moved to the Intensive Care Unit.
Microsurgical Resection Recovery
After the surgery, you will be required to stay in the hospital to recuperate. The length of your hospital stay will vary depending upon several factors including whether there was a rupture, any complications during or after surgery and your general medical condition.
An uncomplicated surgery generally requires a hospital stay of 4 to 6 days, with at least the first day following surgery in the Intensive Care Unit. After release from the hospital, the recovery period at home is three to six weeks for an uncomplicated surgery. Resumption of daily activities, such as driving a car may be as soon as one or two weeks after an uncomplicated surgery where there has been no rupture.
If a rupture occurred during the surgery, a hospital stay of one to two weeks could be expected with a longer initial stay in the Intensive Care Unit. The hospital stay could be longer if complications arise. After release from the hospital, the recovery period at home will vary depending on the specifics of your case.
A follow-up angiogram will usually be performed before release from the hospital to confirm that the AVM has been completely resected.
You should ask your medical team for specific instructions including:
- Restrictions to activity including showering and shampooing
- When to get staples or stitches out
- Necessary follow up appointments
- Anything questions or concerns you have
Possible postoperative symptoms
- Nausea is a reaction that some experience for a short time after general anesthesia. Medications to treat this are available, and you should consult with the anesthesiologist prior to the surgery about them.
- At the incision site itchiness, pain and numbness are common, as well as a clicking noise at the bone reattachment site. These are normal as the incision and the reattached bone section heal. Healing of the bone may take up to six to twelve months.
- Seizures or lapses in consciousness are not common, but if they do occur, medical attention should be sought immediately. Anti-convulsants may be given to prevent seizures.
- Alcohol consumption, which contributes to the possibility of seizures, should be avoided.
- You must not drive a car if you are experiencing seizures, and the law requires that you surrender your driver's license. Once the seizures are eliminated, your doctor will assist you in reclaiming it.
- Memory problems are a common experience and generally improve over time.
- Headaches are a common post-operative experience and can continue for a long time after surgery. They can be treated with medication, and you should consult your physician. After a rupture and treatment, it is highly unlikely that a re-rupture would occur, however, if an extreme or explosive headache does occur, you should seek immediate medical attention.
- Fatigue and tiredness are very common and can continue for six weeks or more.
- Dizziness, confusion, sensitivity to light, and vision or speech impairment sometimes occur. Physical, speech and occupational therapists can assist in dealing with these.
- Constipation sometimes occurs as a result of medications and inactivity and can be treated.
- Back pain from inactivity or lying still can be relieved with medication and physical therapy.
- Depression, fear, anxiety, and anger often occur after experiencing any major surgery or medical emergency. Neurosurgery may affect the problem as well. If you are having difficulty with these feelings it is important to get help from your physician or other medical professionals.

Gamma Knife Machine
You will check into the Gamma Knife program early in the morning on the day of the Radiosurgery procedure. Expect the treatment to take the entire day. Make arrangements to have someone drive you home.
Using sophisticated computer software a Gamma Knife treatment plan will be developed. The information is fed into a computer in the radiosurgery machine showing exactly where the target area is in relation to coordinates. The imaging process and development of treatment plan may take a few hours.
After Radiosurgery you may get swelling in the brain. This can occur within a couple of weeks, or up to a couple of years after treatment. The swelling may cause neurological symptoms or problems. The exact symptoms or problems can vary depending on the location of the treatment. You should consult your physician if you have these symptoms.
Embolization is a non-surgical procedure used to "plug" selected blood vessels to prevent blood flow to the AVM. Embolization is usually supplementary to microsurgical resection. Done prior to microsurgical resection, embolization helps to reduce the size of the AVM by reducing blood flow through the nidus, and/or closing deep feeding blood vessels that may be difficult to gain access to during surgery.
Embolization uses the same procedure as a diagnostic angiogram.
A catheter (a thin hollow tube) is inserted into an artery at the top of the leg. The catheter is monitored as it is guided into place in the targeted blood vessel in the brain. The blood vessel is then "plugged" using various materials. Commonly liquid glue, PVA spheres, or Onyx liquid is used to plug the blood vessel.
When the catheter is in place outside the AVM, the plugging material is injected into the center of the AVM. The materials harden when they come in contact with blood. These materials harden into particles bigger than the diameter of the feeding arteries of the AVM nidus, blocking off blood flow. Bigger vessels may be filled with coils to achieve the same effect. Usually none of these plugging materials have side effects. Usually these substances are removed when the AVM is removed, as embolization is most commonly done in conjunction with microsurgical resection.

Embolization follows the same patient procedure as a diagnostic angiogram, but an embolization procedure will take longer. The embolization procedure will take approximately 3 to 8 hours. Following embolization, you will stay in the Intensive Care Unit for at least an overnight stay. The length of your stay will depend on the specifics of your case.
Following the embolization procedure your Interventional Radiologist will go into specific details about your risks and benefits.
Generally speaking you will be able to go home the next day after completion of the procedure, but that will depend on the specifics of your case.
Embolization is often done in conjunction with microsurgical resection. If that is the case, you will likely be returning for the microsurgical resection within a couple of weeks of the completion of the embolization procedure. If too much time passes between the embolization and the microsurgical resection, the AVM may recruit new blood vessels.
If you develop any neurological symptoms, or your headaches or any other symptoms you have been experiencing get worse, make sure to inform your doctor.
Conservative medical management focuses on monitoring the AVM and relieving associated symptoms. Conservative medical management is usually considered for large AVMs with a Spetzler-Martin (S-M) Grade of 4-5. In patients with a high S-M Grade, the risks of complications from interventional treatment (surgery, or radiosurgery) may be greater than the natural course of the disease.
If you notice any neurological changes, you should notify your doctor as your treatment plan may need to be re-assessed. Particularly if you experience symptoms that indicate the AVM may have ruptured, this should be treated right away. Symptoms of AVM rupture depend on location of the AVM and severity of bleed. Symptoms may include:
- Sudden and severe headache, nausea & vomiting
- Seizure
- Loss of consciousness
- "Stroke-like" symptoms: problems speaking, numbness/tingling, muscle weakness, changes in vision.
Symptom Management
The following are some common symptoms and tactics to help alleviate symptoms. However, you should work with your doctor to determine the best methods to manage symptoms relative to the specifics of your individual case.
Seizures
Seizures can be treated with medications called anti-epileptic drugs (AEDs). Most seizures can be controlled with one or a combination of these medications. Every person is different, so sometimes it takes some trial and error to find the right drug or combination of drugs to control the seizures.
Headaches
For patients with persistent headaches, a CT scan may need to be done to confirm there has not been a bleed. Recognizing and managing headache triggers is key to minimizing headaches. It may be helpful to keep a diary to see if you can determine certain food or environmental allergens that may be causing headaches. Some common headache triggers may include:
- Psychological triggers: stress, anxiety, anger, etc.
- Physical triggers: pressure/swelling from the AVM, poor posture, eye strain, hunger, etc.
- Environmental triggers: allergies to pollen(s), certain foods, smoke, etc.
- Recognizing patterns or factors that cause headaches is essential.
You may need to work closely with a neurologist or a pain specialist if you have debilitating pain. Some general tips:
- Simply rest and relax. Techniques range from deep breathing, to exercising, to meditation and biofeedback. Also, make sure you're getting adequate sleep.
- Good posture, frequent breaks if sitting for long periods of time.
- Sufficient lighting to prevent eye strain, and taking frequent breaks if working on the computer.
- Medication prevention, such as Tylenol.
Because radiation can cause injury to the developing brain, and potentially slow a child's development, radiosurgery is typically not offered to a very young child. Preferably, this treatment option is deferred until a child reaches five years of age. However, as with surgery and embolization, the risks of earlier treatment have to be weighed against the risk of an AVM hemorrhage while waiting for treatment.