Detection of Brain Aneurysms
There has been increasing interest in the detection and treatment of unruptured cerebral aneurysms. Research indicates a higher incidence of aneurysms among family members (highest with siblings). Whether or not relatives should be screened is still controversial, as screening methods have an associated risk and imperfect detection rates. Through routine checkups and recognizing symptoms and causes that are potentially related, one can get the proper screening and scanning needed to diagnose an aneurysm. Special imaging tests are used to detect the presence of a brain aneurysm, some non-invasive to the body, some invasive, and all with differing degrees of risk, accuracy and cost. As of yet, there is no health care insurance coverage for routine aneurysm screening. There are several different diagnostic scans used to locate aneurysms. Your doctor may choose any combination of them based on your particular case and condition.
|
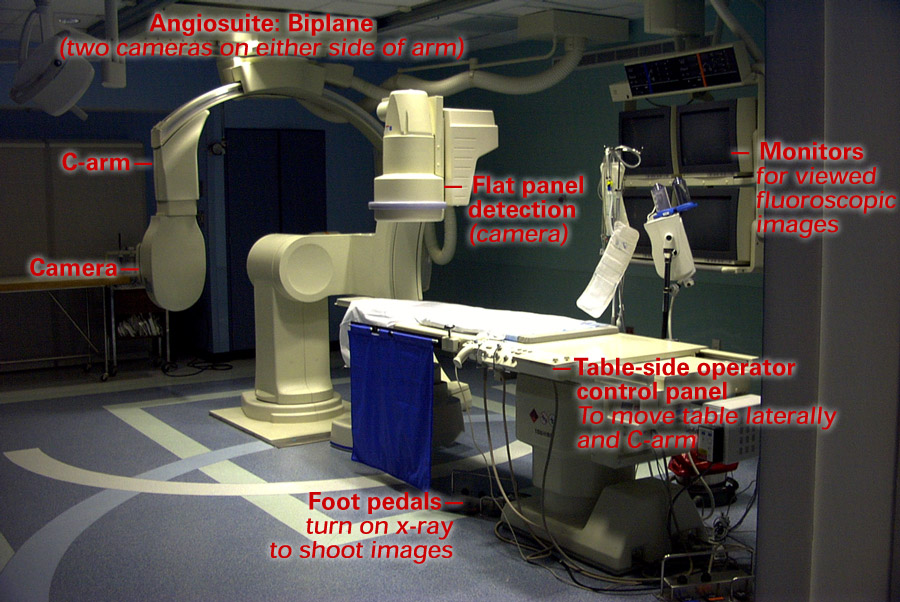
Angiogram (Arteriogram) Angiograms are considered the “gold standard” for diagnostic evaluation of blood vessels because it is the most comprehensive, specific and sensitive. It is however a more expensive and invasive procedure. Because an angiogram is an invasive procedure, we strongly recommend that you go to a neuroradiologist experienced in conducting this type of test to minimize the chance of complications. Review our tips to finding an experienced doctor in our support resources section. You may also hear this test referred to as an arteriogram which references arterial blood vessels specifically. Angiograms are an imaging test using X-Ray pictures to study real-time blood flow. The patient is placed between a steady beam of X-Ray and fluorescent screen. This X-Ray beam and fluorescent screen is a special type of camera called a fluoroscope that enables a continuous running of X-Ray film. The fluoroscope allows your neuroradiologist to watch and record the movement of blood, and to capture single images on X-Ray film.
A contrast agent, or dye, is injected into the blood vessel to increase the visibility of blood flow on the X-Ray pictures. To inject the contrast agent into the blood vessel in the brain, a catheter (a thin hollow tube) is inserted into the artery in the top of the leg. The catheter is then guided to the blood vessel in the brain. The neuroradiologist is able to watch the movement of the catheter with the fluoroscope. Some X-Ray pictures will be taken as the catheter travels up to the brain to help gauge the health of the artery and its ability to carry the catheter to the brain. When the catheter is in place, the contrast agent is injected into the blood vessel and the X-Ray pictures are taken with the fluoroscope. 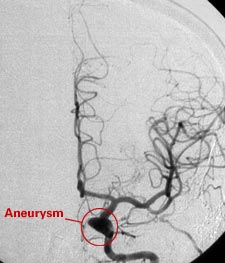 Angiogram done under fluoroscopy. These images are used in angiosuite during a diagnostic or interventional procedure. Courtesy of Dr. Kieran Murphy, Johns Hopkins University, Department of Radiology
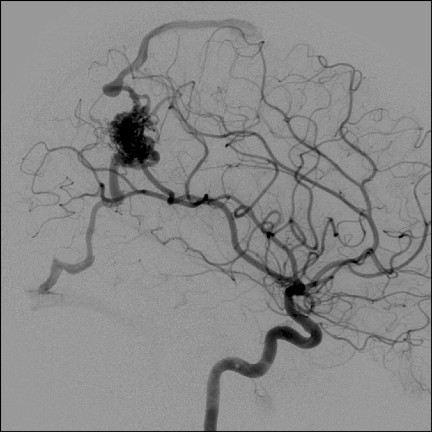
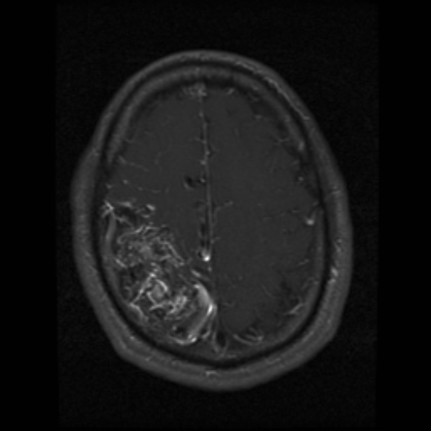
Angiogram of AVM with draining vein Angiogram Patient Procedure You should notify your doctor of any and all medications you are currently taking, as well as any known allergies. Be prepared to bring a list of any current medications, and doses – or if easier bring the pill bottles of all medications you are currently taking. At the time of the test you will change into a hospital gown, and be instructed to remove all jewelry and any other metal objects. You will lie on your back on an X-ray table. Your head and leg where the catheter is inserted may be gently restrained using a strap or tape. This is to aid you in keeping as still as possible while the angiogram is being conducted. A lead apron may be placed under your genital and pelvic areas to protect them from X-Ray exposure. An intravenous (IV) line will be inserted in a vein in your arm. This allows your doctor to dispense medication to calm you if you needed, as well as to dispense fluids to help clear out the contrast agent once the angiogram is completed. A device, called a pulse oximeter, that measures oxygen levels in your blood may be clipped to your finger or ear. Small discs (electrodes) will be placed on your arms, chest, or legs to record your heart rate and rhythm. A round cylinder or rectangular box that takes the pictures during fluoroscopy will be moved above you. The fluoroscope will move under you during the test. You may hear some clicking or whirring noise intermittently throughout the procedure. To prepare for insertion of the catheter into the artery, a small area of your upper thigh (in the groin area) will be shaved and a local anesthetic will be injected. You may feel a brief sting or pinch from the numbing medicine. When the area is numb the neuroradiologist will insert a catheter into the artery at the top of your leg. You may feel pressure in the blood vessel as the catheter is moved. Let your doctor know if you are having pain. Once the catheter is guided to the brain and is in place, the contrast agent will be injected. You may feel a sensation of warmth in your face and head. For some people, the feeling of heat is strong and for others it is very mild. You may also experience headache, flushing of the face, or a salty or metallic taste in your mouth after the dye is used. These feelings do not last long. Some people may feel sick to their stomach or may vomit, but this is uncommon. The dye is an iodine base. If you have a known allergy to iodine or shellfish, notify your doctor as this increases the risk that you may have an allergic reaction to the contrast dye. Alternative dyes may be used, or your doctor may prescribe pre-medications to prevent an allergic reaction to the contrast dye. The contrast dye also holds a small risk of kidney impairment particularly with those over age 65, or with previous kidney or renal problems. Notify your doctor if you have a history of kidney or renal problems. The fluoroscopy equipment will be moved around you into the correct position and pictures will be taken and analyzed by the neuroradiologist. It is important to be as still as possible to obtain clear pictures. You may be asked to take a breath and hold it for several seconds as pictures are being taken. After satisfactory pictures have been obtained, the catheter will be removed and either a closure, or pressure will be applied to the opening for fifteen minutes or more. Following the angiogram you will be required to lie flat for two to six hours in a recovery room at the hospital. Often times patients are administered a medication to help you relax during the procedure. This may interfere with your ability to drive a car, or operate other machinery following the procedure. For this reason, you should be prepared to have someone pick you up and drive you home following the angiogram. Your doctor will give you specific instructions following the test. After the test, you may have some tenderness and bruising at the site where the catheter was inserted. You can use an ice pack on the needle site to relieve any pain and swelling. A diagnostic angiogram takes approximately 2 hours. Risks with an angiogram
|
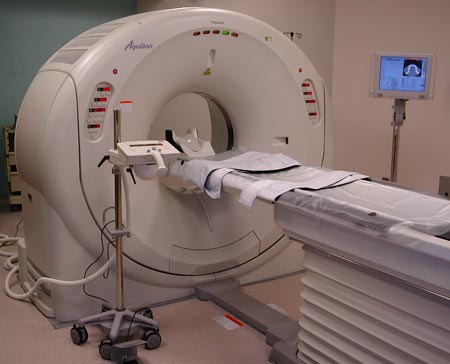
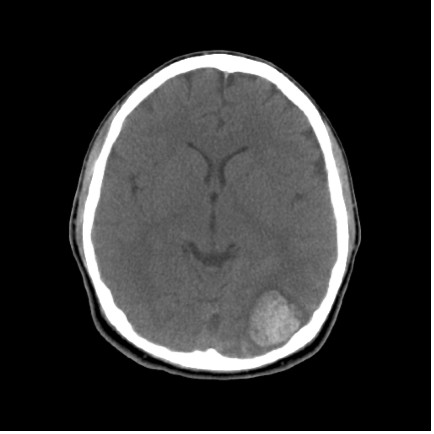
Computed Tomography (CT) Computer Tomography (CT) examines cross-sections of the brain through X-Ray and an interpretive computer. This non-invasive test X-Rays sections of the head in an arc as you are passed through the middle of a donut shaped machine. As the X-Ray beams pass through the body, the density of the tissue determines how the body part is imaged. Bone and blood are very dense, and therefore image very clearly on a CT scan.
To view a video clip of the image, select one of the formats below. in action As a CT scan only captures a flat 2-D slice of the brain (like a piece of paper), usually several scans are done to provide the doctor with layers of anatomical information at different depths.
A related test is a Computer Tomography Angiography (CTA). A CTA augments the CT scan with a contrast dye injected into a vein in the arm, which allows for 3-D imaging highlighting the blood vessels in the brain. CT/CTA Patient Procedure With a CTA test, you will be injected in a vein in the arm with a contrast dye prior to the CT scan. You may have a headache, flushing of the face, or a salty or metallic taste in your mouth after the dye is used. These feelings do not last long. Some people may feel sick to their stomach or may vomit, but this is uncommon. The dye is an iodine base. If you have a known allergy to iodine or shellfish, notify your doctor as this increases the risk that you may have an allergic reaction to the contrast dye. Alternative dyes may be used, or your doctor may prescribe pre-medications to prevent an allergic reaction to the contrast dye. The contrast dye also holds a small risk of kidney impairment particularly with those over age 65, or with previous kidney or renal problems. Notify your doctor if you have a history of kidney or renal problems.
|
One limiting factor for broad-based population screening is the logistical and financial burden. One study in Ireland examines the costs associated with screening first degree relatives (parents, siblings and children) 18-65 years with a history of family intracranial aneurysms (IA) (Roberts et al., Screening for familial intracranial aneurysm: resource implications. Br J Neurosurg. 1999 Aug;13(4):395-8). A study screening first-degree relatives in Northern Ireland found a 15% yield. This translates to finding 700 asymptomatic patients with intracranial aneurysms in a national screening of the population of Northern Ireland. The time it would take to screen the population once would be 2.3 years by catheter angiogram, and 1.1 years by magnetic resonance angiography (MRA). Unfortunately, the study does not take into account the treatment cost should those undiscovered aneurysms rupture. Another study (Raaymakers et al), Aneurysms in relatives of patients with subarachnoid hemorrhage: frequency and risk factors. MARS Study Group. Magnetic Resonance Angiography in Relatives of patients with Subarachnoid hemorrhage, Neurology. 1999 Sep 22;53(5):982-8) cites the incidence of IA (MRA diagnosis) in first-degree relatives of SAH patients as 4.0%, with female gender, increasing age, polycystic kidney disease, hypertension and elevated levels of glucose and cholesterol in the blood as risk factors. Atheroscelerosis, smoking, alcohol use or a previous history of SAH, were not significant factors. One study, from 1996, shows that 80% of familial aneurysms occurred in women versus the 59% of sporadic aneurysms among women (LeBlanc, Familial Cerebral Aneursyms, Stroke. 1996 Jun;27(6):1050-4). Clearly more research is needed to determine the utility of more widespread screening. |